Caring for your affected child’s physical health
Since transplant, you are probably acutely aware of your child’s physical health. You may feel like you are constantly monitoring for any signs of complications, such as fevers, skin infections, or rashes, or signs of graft-versus-host disease or an adrenal crisis, to name a few. It will continue to be important to attend regular check-ups with your child’s medical team, and to let them know if you have any new concerns.
Adequate sleep, nutrition, and physician-approved physical activity will also go a long way in helping your child feel their best. If you are concerned about your child’s sleep, nutrition, or energy levels, bring this up to your child’s doctor. There may be some simple solutions to help improve your child’s sleep quality or stimulate their appetite. There also may be other underlying reasons that your child is having these difficulties that can be assessed further, such as hormone imbalances, depression, or anxiety.
Since transplant, you are probably acutely aware of your child’s physical health. You may feel like you are constantly monitoring for any signs of complications, such as fevers, skin infections, or rashes, or signs of graft-versus-host disease or an adrenal crisis, to name a few. It will continue to be important to attend regular check-ups with your child’s medical team, and to let them know if you have any new concerns.
Adequate sleep, nutrition, and physician-approved physical activity will also go a long way in helping your child feel their best. If you are concerned about your child’s sleep, nutrition, or energy levels, bring this up to your child’s doctor. There may be some simple solutions to help improve your child’s sleep quality or stimulate their appetite. There also may be other underlying reasons that your child is having these difficulties that can be assessed further, such as hormone imbalances, depression, or anxiety.
Nicholas is finally free from his hospital lines for the first time in a month.
Watch him celebrate!
Watch him celebrate!
Caring for your affected child’s mental health
Every child has their own unique way of coping while recovering from transplant. Their ability to cope is also impacted by different factors, including whether they experience significant complications, physical limitations, or social or emotional challenges. Some children may have already struggled with low mood, anxiety, behavioral challenges, academic, or social difficulties even before transplant, and therefore need continued support. There is no “one size fits all” approach to helping your child adjust to life after transplant. You know your child best and will be the best person to identify whether there have been any noticeable changes in your child after treatment that may require additional support.
Behavioral Health Services
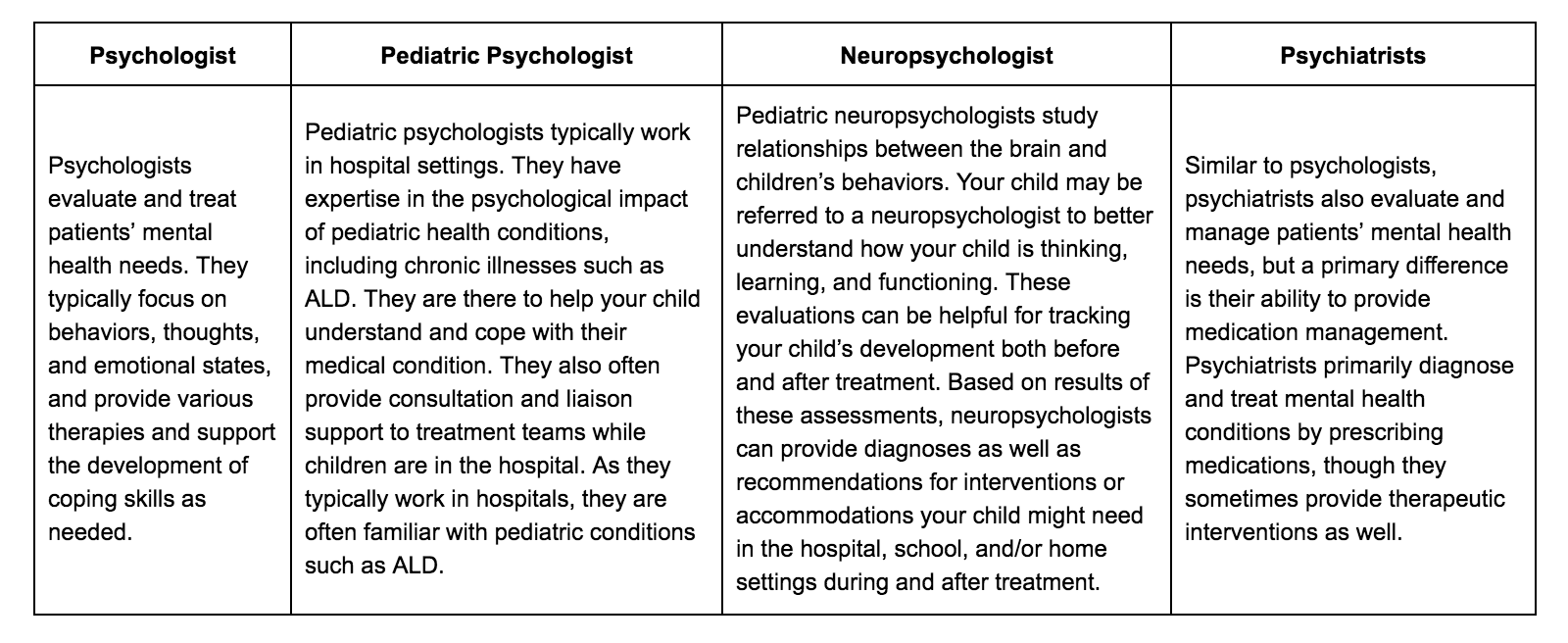
If you are concerned that your child is having difficulty in school, with friends, or they are showing signs of emotional or behavioral difficulties (e.g., depression, irritability, anxiety, outbursts, inattention, hyperactivity), we recommend reaching out to some local mental health providers to see if they have any available appointments or to get on a waitlist. Although some symptoms may resolve when children are able to resume school or other activities, your child’s symptoms may not go away on their own, and therapy or medications may help your child feel better and cope with their current circumstances. There are a variety of behavioral health resources that may be available in your area, which include psychologists, pediatric psychologists, neuropsychologists, and psychiatrists. The four professions sound similar, but have key differences.
Psychology Today can be helpful for locating a provider in your area, or you can always contact your insurance carrier to find out which providers work with children and are in-network and accepting new patients. You can also reach out to your child’s medical team to ask about potential referrals in your area.
In addition to providers in your local community, your child may also be able to receive support for their social, emotional, and behavioral functioning in school. Reach out to your child’s teacher or school administrators to find out if your child has a school psychologist, social worker, or a counselor on staff who can provide additional support for your child in the school setting.
School Psychologists
School psychologists promote positive learning environments for students by addressing academic, social, emotional, and behavioral needs. They are certified professionals trained to administer psychological and academic assessments to evaluate students’ needs within the educational setting. They make recommendations, implement evidence-based prevention and intervention programs, monitor progress, and equip students with the skills and tools needed to thrive in the classroom. School psychologists communicate with parents and teachers frequently to provide updates on student progress. They are also trained to work with diverse populations to create developmentally- and culturally-appropriate plans.
School Social Workers
Similar to school psychologists, school social workers also address students’ academic, social, emotional, and behavioral needs. While school psychologists have more expertise in special education and implementing assessments and programs in school settings, school social workers focus more on student’s success and well-being in and outside of school. They may provide individual and group therapy or counseling in the school setting. They also act as a liaison between students, parents, teachers, school staff, and the community. They work closely with students and families to assist with community referrals, home support resources, finances, transitioning from home to school, and long-term case management.
School Counselors
School counselors are certified/licensed educators who work in elementary, middle school, and high schools to support efforts to improve student success and outcomes. They develop and implement a school counseling program so that all students can thrive. In addition, they help students achieve their academic, personal, and career goals. They may offer short-term counseling services, collaborate with teachers, parents, and administrators to meet students’ needs, help students individually with academic planning and goal setting, and advocate for changes to improve equity and access to opportunities for all students.
In addition to providers in your local community, your child may also be able to receive support for their social, emotional, and behavioral functioning in school. Reach out to your child’s teacher or school administrators to find out if your child has a school psychologist, social worker, or a counselor on staff who can provide additional support for your child in the school setting.
School Psychologists
School psychologists promote positive learning environments for students by addressing academic, social, emotional, and behavioral needs. They are certified professionals trained to administer psychological and academic assessments to evaluate students’ needs within the educational setting. They make recommendations, implement evidence-based prevention and intervention programs, monitor progress, and equip students with the skills and tools needed to thrive in the classroom. School psychologists communicate with parents and teachers frequently to provide updates on student progress. They are also trained to work with diverse populations to create developmentally- and culturally-appropriate plans.
School Social Workers
Similar to school psychologists, school social workers also address students’ academic, social, emotional, and behavioral needs. While school psychologists have more expertise in special education and implementing assessments and programs in school settings, school social workers focus more on student’s success and well-being in and outside of school. They may provide individual and group therapy or counseling in the school setting. They also act as a liaison between students, parents, teachers, school staff, and the community. They work closely with students and families to assist with community referrals, home support resources, finances, transitioning from home to school, and long-term case management.
School Counselors
School counselors are certified/licensed educators who work in elementary, middle school, and high schools to support efforts to improve student success and outcomes. They develop and implement a school counseling program so that all students can thrive. In addition, they help students achieve their academic, personal, and career goals. They may offer short-term counseling services, collaborate with teachers, parents, and administrators to meet students’ needs, help students individually with academic planning and goal setting, and advocate for changes to improve equity and access to opportunities for all students.
Monitoring your child’s neuropsychological functioning
Periodic monitoring of your child’s neuropsychological functioning by a pediatric neuropsychologist may be offered as part of the comprehensive care for individuals with ALD at a specialty center. Before your child underwent transplant, your child may have had a baseline neuropsychological assessment (e.g., an estimate of your child’s neuropsychological functioning before treatment). Routine follow-up evaluations, which usually happen once per year or as requested by your child’s medical team, are often standard of care for cerebral ALD. These evaluations are helpful for tracking your child’s progress over time and identifying any areas where your child may need additional support.
While some individuals with cerebral ALD show very few or only subtle challenges following treatment, especially if they were treated at an early stage of the disease, other individuals may experience changes in a number of different areas. Research has found that the most common areas of difficulty for individuals with cerebral ALD include: speed of processing information; perceiving, organizing, interpreting and thinking with visual information; navigating one’s environment and where objects are in space; balance and coordination; moving fingers quickly to perform tasks; focus and concentration; managing impulses and activity level; and managing thoughts, emotions, and behaviors. Sometimes, areas of difficulty emerge at home, while other times, they become more apparent as your child returns to school. For many individuals, the treatment process itself can be quite scary, overwhelming, and isolating, which can lead to feelings of anxiety, sadness, loneliness, and even trauma that were not present before treatment. You may notice some changes in your child’s emotions and behavior after treatment, while other parents/caregivers report that their child seems “shut down” or “withdrawn” and is hesitant to share their feelings. It is not uncommon for children to share more worries or become angry or tearful more often. For this reason, it is important to check in regularly with those who interact with and spend the most time with your child (e.g., their teachers, coaches, counselors, etc.) to identify any new concerns as they arise.
Unfortunately, it is difficult to predict how your child will function in terms of their patterns of strengths and weaknesses following treatment. Outcomes differ from one individual to the next. These differences can be due to several factors, including the degree of disease progression prior to transplant, the location of the disease in the brain (e.g., parietal/occipital versus frontal regions of the brain), and how the individual functioned prior to transplant. It can also take some time for your child’s brain to stabilize after treatment. This means that new areas of concern may emerge as more time has passed since treatment. For this reason, it is important for your child’s neuropsychological functioning to be monitored over time, at least for the first few years after treatment. This will ensure that appropriate support and accommodations can be provided to meet your child’s areas of need.
Periodic monitoring of your child’s neuropsychological functioning by a pediatric neuropsychologist may be offered as part of the comprehensive care for individuals with ALD at a specialty center. Before your child underwent transplant, your child may have had a baseline neuropsychological assessment (e.g., an estimate of your child’s neuropsychological functioning before treatment). Routine follow-up evaluations, which usually happen once per year or as requested by your child’s medical team, are often standard of care for cerebral ALD. These evaluations are helpful for tracking your child’s progress over time and identifying any areas where your child may need additional support.
While some individuals with cerebral ALD show very few or only subtle challenges following treatment, especially if they were treated at an early stage of the disease, other individuals may experience changes in a number of different areas. Research has found that the most common areas of difficulty for individuals with cerebral ALD include: speed of processing information; perceiving, organizing, interpreting and thinking with visual information; navigating one’s environment and where objects are in space; balance and coordination; moving fingers quickly to perform tasks; focus and concentration; managing impulses and activity level; and managing thoughts, emotions, and behaviors. Sometimes, areas of difficulty emerge at home, while other times, they become more apparent as your child returns to school. For many individuals, the treatment process itself can be quite scary, overwhelming, and isolating, which can lead to feelings of anxiety, sadness, loneliness, and even trauma that were not present before treatment. You may notice some changes in your child’s emotions and behavior after treatment, while other parents/caregivers report that their child seems “shut down” or “withdrawn” and is hesitant to share their feelings. It is not uncommon for children to share more worries or become angry or tearful more often. For this reason, it is important to check in regularly with those who interact with and spend the most time with your child (e.g., their teachers, coaches, counselors, etc.) to identify any new concerns as they arise.
Unfortunately, it is difficult to predict how your child will function in terms of their patterns of strengths and weaknesses following treatment. Outcomes differ from one individual to the next. These differences can be due to several factors, including the degree of disease progression prior to transplant, the location of the disease in the brain (e.g., parietal/occipital versus frontal regions of the brain), and how the individual functioned prior to transplant. It can also take some time for your child’s brain to stabilize after treatment. This means that new areas of concern may emerge as more time has passed since treatment. For this reason, it is important for your child’s neuropsychological functioning to be monitored over time, at least for the first few years after treatment. This will ensure that appropriate support and accommodations can be provided to meet your child’s areas of need.